 In previous posts, we’ve already talked about what Clinical Reasoning is and why it is important. We’ve explored as well how Clinical Reasoning and Critical Thinking are intimately tied together. Now, let’s talk about the clinical reasoning process.
In previous posts, we’ve already talked about what Clinical Reasoning is and why it is important. We’ve explored as well how Clinical Reasoning and Critical Thinking are intimately tied together. Now, let’s talk about the clinical reasoning process.
A concept called the Clinical Reasoning Cycle, promoted by Tracy-Levett Jones, a professor of Nursing at Newcastle, organizes the clinical reasoning process into several steps. It walks every healthcare professional, especially physicians and nurses, through systematic steps that involve logical considerations. Adopting this cycle facilitates the “thinking” behind the patient’s management plan, allowing the healthcare professional to go through a series of systematic phases, ultimately leading to a final decision that considers what is best for the patient in a particular situation.
Various Phases of the Clinical Reasoning Cycle
There are eight phases of clinical reasoning and one must note that this process, though divided into phases, is a continuum. In reality, one does not always move from one step or phase to the next, but rather move back and forth from one phase to another until an accurate assessment of a patient’s health status is made.
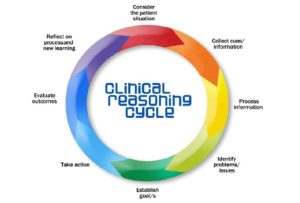
Adapted from Tracy Levett-Jones, et al. (2010)
The various phases of clinical reasoning include:
Consideration of facts from the patient or situation
This is the phase where you are first presented with a clinical case. Here you receive the presenting information and current medical status of the patient, for example, a new-born admitted in the NICU on account of neonatal jaundice.
Collection of information
In this phase, you carefully consider the past medical history of the patient, the history of presenting complaints, the current treatment plan, results of investigations done, and current vital signs. You then analyse the findings using your established knowledge of physiology, pharmacology, pathology, culture, and ethics to establish cues and draw information.
Processing gathered information
This is a critical stage and the core of clinical reasoning. Here, you process the data on the patient’s current health status in relation to pathophysiological and pharmacological patterns, know what details are relevant, and determine potential outcomes for possible decisions you make.
Identify the problem
With a solid information processing phase, you will be able to determine the reason behind the patient’s current state.
Establish goals
Here, you determine the treatment goals for the patient’s situation.Treatment plans should not be open-ended or without a time-oriented goal. Know what step to take, and how fast you want the desired outcome.
Take action
Now, you implement the actions steps needed to meet the patient’s treatment goals. This will, of course, involve other members of the healthcare team, so everyone should be updated about the treatment goals for the particular patient.
Evaluation
At this phase, you evaluate the effectiveness of the course of action you have taken. This will allow you to determine whether to readjust or continue the line of action.
Reflection
This phase of clinical reasoning fortifies the skill. At this phase, you reflect on new things you learned about the case, what you could have done differently to achieve a better outcome, and what should be avoided in similar occurrences in the future.
Following these phases of the clinical reasoning cycle will facilitate problem-solving and decision making, allowing you as a health care professional to provide the best care for your patients.







